At the University of Florida’s Wertheim UF Scripps Institute for Biomedical Innovation and Technology, a research team led by Professor Patrick Griffin, scientific director and molecular biologist, has developed a new group of experimental compounds designed to reprogram insulin resistant cells toward healthier metabolic behavior. The work focuses on improving insulin sensitivity while reducing the side effects that have limited the long term use of earlier diabetes medications.
Kuo, K.-T., Bdiri, B., He, Y., Garcia-Ordonez, R. D., McDougal, D. P., Ruiz, C., Chang, M. R., Cameron, M. D., Bruning, J. B., Kamenecka, T. M., & Griffin, P. R. (2025). Structural determinants of non-covalent PPARγ inverse agonism and their therapeutic implications. Nature Communications. https://doi.org/10.1038/s41467-025-67608-5
Type 2 diabetes affects millions of people worldwide and develops when cells no longer respond effectively to insulin. This dysfunction prevents glucose from being properly absorbed and metabolized, leading to elevated blood sugar levels and long term damage to organs and tissues. Many patients with type 2 diabetes also suffer from chronic kidney disease or cardiovascular conditions, which restrict the range of treatments they can safely receive.
University of Florida’s, Professor Patrick Griffin stated,
“With 26 compounds and three independent simulations per compound, the total computing time approached 20 days. Future studies will explore how downstream molecules interact with the PPAR gamma-targeting compounds. Seeing this research accelerate in ways that directly address urgent patient needs is deeply gratifying. We’re committed to translating these findings into clinical progress.”
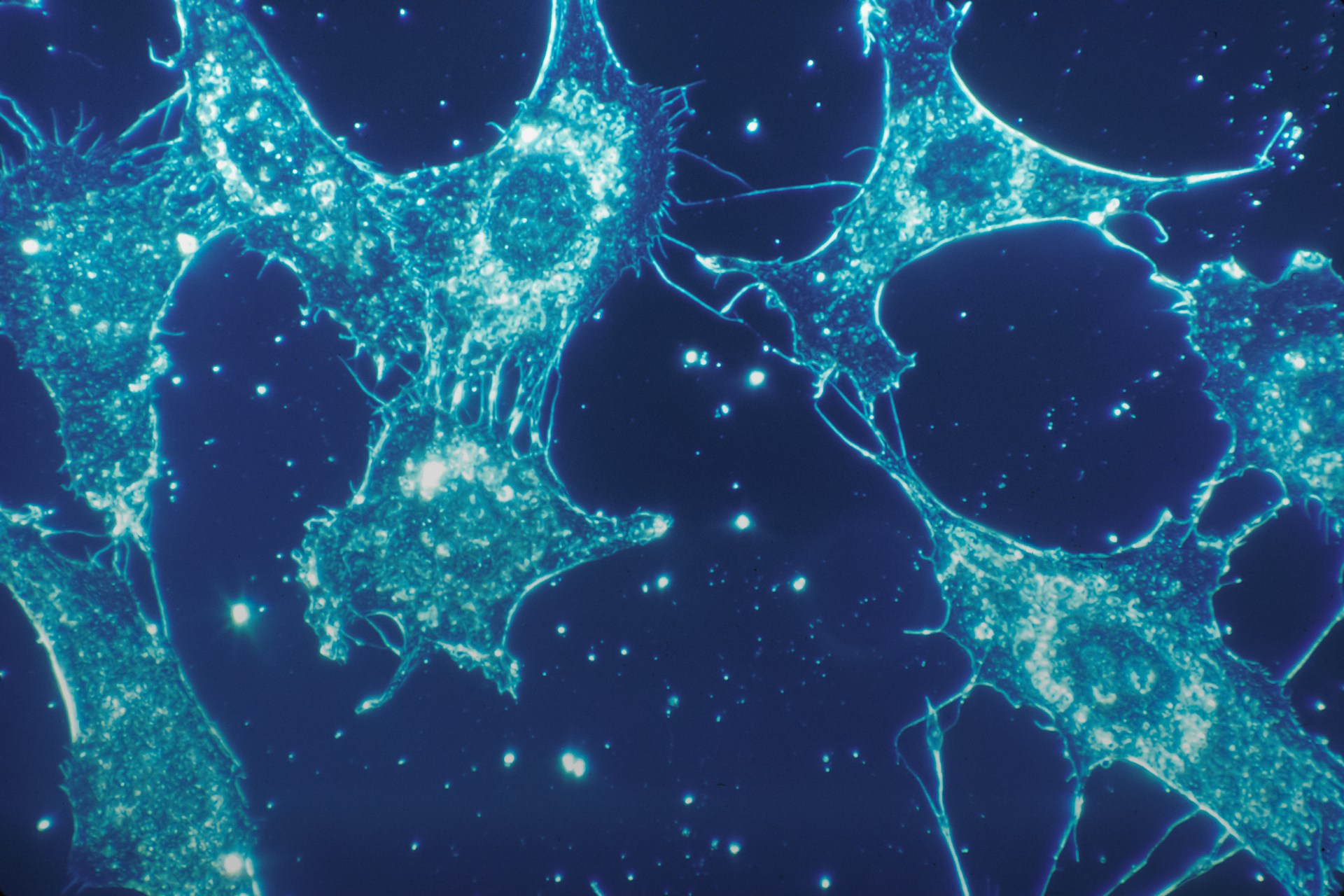
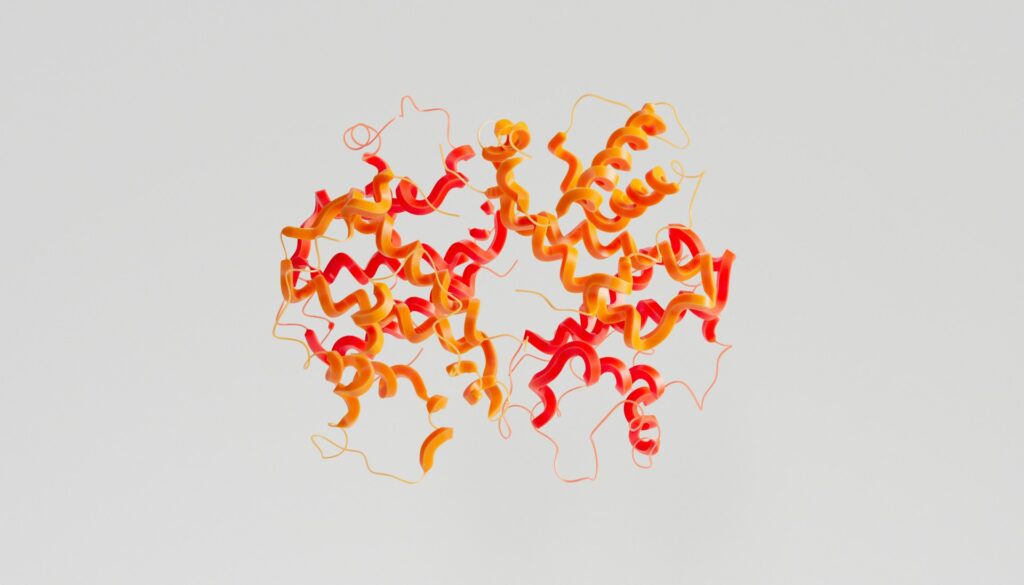
The research centers on PPAR gamma, a nuclear receptor that regulates fat cell development, glucose metabolism, and insulin signaling. Because PPAR gamma directly interacts with DNA to control gene expression, it has long been viewed as a powerful therapeutic target. At the same time, its involvement in multiple biological systems has made it difficult to manipulate without triggering harmful side effects.
Earlier medications targeting PPAR gamma, commonly known as glitazones, demonstrated strong improvements in insulin sensitivity but were later linked to adverse outcomes affecting the heart, bones, and fluid balance. These risks led to strict regulatory warnings and a decline in their clinical use. Rather than abandoning the target, Griffin’s team sought to understand how to modulate PPAR gamma activity in a more controlled manner.
To do this, the researchers combined computational modeling, structural analysis, and laboratory testing. Medicinal chemist Theodore Kamenecka collaborated with the group to design compounds capable of interacting with PPAR gamma in a way that alters its signaling behavior without fully activating it. Graduate researcher Kuang Ting Kuo played a key role in integrating data across modeling and experimental platforms.
Advanced computer simulations were used to study how different compounds influence the shape and flexibility of the PPAR gamma protein. These simulations were paired with biochemical assays and hydrogen deuterium exchange mass spectrometry, a technique that reveals subtle structural changes in proteins as they interact with small molecules. Together, these methods allowed the team to predict how specific chemical features would affect biological outcomes.
After identifying promising candidates, the researchers tested the compounds in mouse and human fat cells. The results showed that several compounds improved insulin sensitivity while avoiding patterns of gene activation associated with known side effects. Rather than acting as strong activators, the compounds appeared to fine tune PPAR gamma signaling, encouraging healthier metabolic function at the cellular level.
This approach reflects a broader shift in drug design toward selective modulation of complex signaling proteins. Instead of maximizing receptor activation, engineers and biologists are increasingly focused on guiding receptors toward specific functional states that provide therapeutic benefit with fewer unintended consequences.
The research team notes that the compounds are still in early stages of development. Further studies will be needed to evaluate how they behave across different tissues and in more complex biological systems. Understanding these interactions will be essential before any clinical testing can take place.
Beyond diabetes, the study demonstrates how modern drug discovery relies on integrating computational power with experimental validation. By using simulations to narrow down viable candidates before extensive laboratory testing, researchers aim to reduce development time and improve safety profiles.
For patients with limited treatment options due to coexisting conditions, the findings point toward a potential future in which insulin sensitivity can be improved without exposing vulnerable populations to excessive risk. From an engineering perspective, the work highlights how precise molecular design can reshape how cells respond to long standing therapeutic targets.

Adrian graduated with a Masters Degree (1st Class Honours) in Chemical Engineering from Chester University along with Harris. His master’s research aimed to develop a standardadised clean water oxygenation transfer procedure to test bubble diffusers that are currently used in the wastewater industry commercial market. He has also undergone placments in both US and China primarely focused within the R&D department and is an associate member of the Institute of Chemical Engineers (IChemE).